Thyroid cancer
| Thyroid cancer | |
|---|---|
 | |
| Micrograph of a papillary thyroid carcinoma demonstrating diagnostic features (nuclear clearing and overlapping nuclei). | |
| Specialty | Oncology |
| Symptoms | Swelling or lump in the neck[1] |
| Risk factors | Radiation exposure, enlarged thyroid, family history,[1][2] obesity[3] |
| Diagnostic method | Ultrasound, fine needle aspiration[1] |
| Differential diagnosis | Thyroid nodule, metastatic disease[1][4] |
| Treatment | Surgery, radiation therapy, chemotherapy, thyroid hormone, targeted therapy, watchful waiting[1] |
| Prognosis | Five year survival rates 98% (US)[5] |
| Frequency | 3.2 million (2015)[6] |
| Deaths | 31,900 (2015)[7] |
Thyroid cancer is cancer that develops from the tissues of the thyroid gland.[1] It is a disease in which cells grow abnormally and have the potential to spread to other parts of the body.[8][9] Symptoms can include swelling or a lump in the neck, difficulty swallowing or voice changes including hoarseness, or a feeling of something being in the throat due to mass effect from the tumor. However, most cases are asymptomatic.[1][10] Cancer can also occur in the thyroid after spread from other locations, in which case it is not classified as thyroid cancer.[4]
Risk factors include radiation exposure at a young age, having an enlarged thyroid, family history and obesity.[1][2][3] The four main types are papillary thyroid cancer, follicular thyroid cancer, medullary thyroid cancer, and anaplastic thyroid cancer.[4] Diagnosis is often based on ultrasound and fine needle aspiration.[1] Screening people without symptoms and at normal risk for the disease is not recommended.[10][11]
Treatment options may include surgery, radiation therapy including radioactive iodine, chemotherapy, thyroid hormone, targeted therapy, and watchful waiting.[1] Surgery may involve removing part or all of the thyroid.[4] Five-year survival rates are 98% in the United States.[5]
Globally as of 2015, 3.2 million people have thyroid cancer.[6] In 2012, 298,000 new cases occurred.[12] It most commonly is diagnosed between the ages of 35 and 65.[5] Women are affected more often than men.[5] Those of Asian descent are more commonly affected;[4] with a higher rate of mortality among Filipino females.[13] Rates have increased in the last few decades, which is believed to be due to better detection.[12] In 2015, it resulted in 31,900 deaths.[7]
Signs and symptoms
[edit]Most people with thyroid cancer do not have symptoms at the time of diagnosis and thyroid nodules and thyroid cancer is usually found incidentally on imaging of the neck.[10][14] Up to 65% of adults have small nodules in their thyroids, but typically under 10% of these nodules are found to be cancerous.[15] Sometimes, the first sign is an enlarged lymph node. Later symptoms that can be present are pain in the anterior region of the neck and changes in voice due to an involvement of the recurrent laryngeal nerve.[16]
Thyroid cancer is usually found in a euthyroid patient, but symptoms of hyperthyroidism or hypothyroidism may be associated with a large or metastatic, well-differentiated tumor. Thyroid nodules are of particular concern when they are found in those under the age of 20. The presentation of benign nodules at this age is less likely, thus the potential for malignancy is far greater.[17]
Causes
[edit]Thyroid cancers are thought to be related to a number of environmental and genetic predisposing factors, but significant uncertainty remains regarding their causes.[18]
Environmental exposure to ionizing radiation from both natural background sources and artificial sources is suspected to play a significant role, and significantly increased rates of thyroid cancer occur in those exposed to mantlefield radiation for lymphoma, and those exposed to iodine-131 following the Chernobyl,[19] Fukushima, Kyshtym, and Windscale[20] nuclear disasters.[21] Thyroiditis and other thyroid diseases also predispose to thyroid cancer.[20][22]
Genetic causes include multiple endocrine neoplasia type 2, which markedly increases rates, particularly of the rarer medullary form of the disease.[23] Mutations in the genes for MenA and Men2B in multiple endocrine neoplasia is responsible for 25% of medullary thyroid cancers.[10]
Diagnosis
[edit]
After a thyroid nodule is found during a physical examination or incidentially on imaging, a referral to an endocrinologist or a thyroidologist may occur. Most commonly, an ultrasound is performed to confirm the presence of a nodule and assess the status of the whole gland. Various radiological clinical criteria, including the thyroid imaging reporting and data system (TIRADs) score, are used to characterize the risk of malignancy.[24] On ultrasound, nodules that are hypoechogenic (solid consistency), having irregular borders, increased vascularity, calcifications, or being taller than wide on transverse views are associated with malignancy.[10] Biopsy or cytology are required if the ultrasound characteristics suggest malignancy. If ultrasound results are equivocal or unclear, or if the thyroid nodule is small (typically less than 1 cm), the nodule can be monitored over time with serial ultrasounds.[10] Ultrasound has a sensitivity of 64-77% and a specificity of 82-90% for the detection of thyroid cancer.[10] Measurement of thyroid stimulating hormone, free and/or total triiodothyronine (T3) and thyroxine (T4) levels, and antithyroid antibodies will help decide if a functional thyroid disease such as Hashimoto's thyroiditis is present, a known cause of a benign nodular goiter.[25] A thyroid scan, performed often in conjunction with a radioactive iodine uptake test may be used to determine whether a nodule is hyperactive[26] which may help to make a decision whether to perform a biopsy of the nodule.[27] Measurement of calcitonin is necessary to exclude the presence of medullary thyroid cancer. To achieve a definitive diagnosis, a fine needle aspiration cytology test may be performed and reported according to the Bethesda system.[28]
After diagnosis, to understand potential for spread of disease, or for follow up monitoring after surgery, a whole body I-131 or I-123 radioactive iodine scan may be performed.[29]
In adults without symptoms, screening for thyroid cancer is not recommended.[30]
Classification
[edit]
Thyroid cancers can be classified according to their histopathological characteristics.[32][33] These variants can be distinguished (distribution over various subtypes may show regional variation):
- Papillary thyroid cancer (75 to 85% of cases[34]) – is more often diagnosed in young females compared to other types of thyroid cancer and has an excellent prognosis. It may occur in women with familial adenomatous polyposis and in patients with Cowden syndrome. A follicular variant of papillary thyroid cancer also exists.[35]
- Newly reclassified variant: noninvasive follicular thyroid neoplasm with papillary-like nuclear features is considered an indolent tumor of limited biologic potential.
- Follicular thyroid cancer (10 to 20% of cases[34]) – occasionally seen in people with Cowden syndrome. Some include Hürthle cell carcinoma as a variant and others list it as a separate type.[4][36]
- Medullary thyroid cancer (5[34] to 8% of cases) – cancer of the parafollicular cells, often part of multiple endocrine neoplasia type 2.[37]
- Poorly differentiated thyroid cancer
- Anaplastic thyroid cancer (1 to 2%[38]) despite constituting only 1% of thyroid cancers, the type is responsible for 20% of thyroid cancer deaths.[10] It is characterized by a severe course with median survival of 6.5 months.[10]
- Others
The follicular and papillary types together can be classified as "differentiated thyroid cancer".[39] These types have a more favorable prognosis than the medullary and undifferentiated types.[40]
- Papillary microcarcinoma is a subset of papillary thyroid cancer defined as a nodule measuring less than or equal to 1 cm.[41] 43% of all thyroid cancers and 50% of new cases of papillary thyroid carcinoma are papillary microcarcinoma.[42][43] Management strategies for incidental papillary microcarcinoma on ultrasound (and confirmed on FNAB) range from total thyroidectomy with radioactive iodine ablation to lobectomy or observation alone. Harach et al. suggest using the term "occult papillary tumor" to avoid giving patients distress over having cancer. Woolner et al. first arbitrarily coined the term "occult papillary carcinoma", in 1960, to describe papillary carcinomas ≤ 1.5 cm in diameter.[44]
Staging
[edit]Cancer staging is the process of determining the extent of the development of a cancer. The TNM staging system is usually used to classify stages of cancers, but not of the brain.[45]
-
Stage M1 thyroid cancer
-
Stage N1a thyroid cancer
-
Stage N1b thyroid cancer
-
Stage T1a thyroid cancer
-
Stage T1b thyroid cancer
-
Stage T2 thyroid cancer
-
Stage T3 thyroid cancer
-
Stage T4a thyroid cancer
-
Stage T4b thyroid cancer
Metastases
[edit]Detection of differentiated thyroid cancer metastases may be detected by performing a full-body scintigraphy using iodine-131.[46][47]
Spread
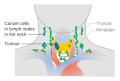
[edit]Thyroid cancer can spread directly, via lymphatics or blood. Direct spread occurs through infiltration of the surrounding tissues. The tumor infiltrates into infrahyoid muscles, trachea, oesophagus, recurrent laryngeal nerve, carotid sheath, etc. The tumor then becomes fixed. Anaplastic carcinoma spreads mostly by direct spread, while papillary carcinoma spreads so the least. Lymphatic spread is most common in papillary carcinoma. Cervical lymph nodes become palpable in papillary carcinoma even when the primary tumor is unpalpable. Deep cervical nodes, pretracheal, prelaryngeal, and paratracheal groups of lymph nodes are often affected. The lymph node affected is usually the same side as that of the location of the tumor. Blood spread is also possible in thyroid cancers, especially in follicular and anaplastic carcinoma. The tumor emboli do angioinvasion of lungs; end of long bones, skull, and vertebrae are affected. Pulsating metastases occur because of their increased vascularity.[48]
Treatment
[edit]Thyroidectomy and dissection of central neck compartment is the initial step in treatment of thyroid cancer in the majority of cases.[14] Thyroid-preserving operations may be applied in cases, when thyroid cancer exhibits low biological aggressiveness (e.g. well-differentiated cancer, no evidence of lymph-node metastases, low MIB-1 index, no major genetic alterations like BRAF mutations, RET/PTC rearrangements, p53 mutations etc.) in patients younger than 45 years.[49] If the diagnosis of well-differentiated thyroid cancer (e.g. papillary thyroid cancer) is established or suspected by FNA, then surgery is indicated.[49][50] Surgical resection is the preferred treatment for all biopsy confirmed thyroid cancers. In those with very low risk tumors (such as small papillary tumors without evidence of local or metastatic spread or concerning cytologic findings), patients at high surgical risk due to medical problems, those with short expected lifespans or patients with serious medical issues precluding surgery, an active surveillance approach, in which the tumor is monitored over time (such as with serial imaging) may be pursued.[51]
Post surgical monitoring for recurrence or metastasis may include routine ultrasound, CT scans, FDG-PET/CT, radioactive iodine whole body scans, and routine laboratory blood tests for changes in thyroglobulin, thyroglobulin antibodies, or calcitonin, depending on the subtype of thyroid cancer.[52][53][54]
Radioactive iodine-131 is used in people with papillary or follicular thyroid cancer for ablation of residual thyroid tissue after surgery and for the treatment of thyroid cancer.[55] Post-surgical radioactive iodine is recommended for those with high risk of cancer recurrence. Post-surgery radioactive iodine does not reduce recurrence in those with low risk thyroid cancer.[10] Patients with medullary, anaplastic, and most Hurthle-cell cancers do not benefit from this therapy.[14] External irradiation may be used when the cancer is unresectable, when it recurs after resection, or to relieve pain from bone metastasis.[14]
Sorafenib and lenvatinib are approved for advanced metastatic thyroid cancer.[56] Numerous agents are in phase II and III clinical trials.[56]
Prognosis
[edit]This section needs additional citations for verification. (October 2014) |
The prognosis of thyroid cancer is related to the type of cancer and the stage at the time of diagnosis. For the most common form of thyroid cancer, papillary, the overall prognosis is excellent.
Many small thyroid cancers (mostly papillary type) rarely grow or metastasize. Some have stated that thyroid cances are overdiagnosed and will rarely cause symptoms, illness, or death, even without treatment.[57] Low grade thyroid cancer is very commonly seen during autopsy studies, with the person dying from other causes.[57] Increasingly, small thyroid nodules are discovered as incidental findings on imaging (CT scan, MRI, ultrasound) performed for another purpose. Few of these people with incidentally discovered, subclinical thyroid cancers will ever have any symptoms, and overtreatment may be present.[57]
Thyroid cancer is three times more common in women than in men.[58] The overall relative 5-year survival rate for thyroid cancer is 85% for females and 74% for males.[59]
The table below highlights some of the 5 and 10 year survival rates of various types of thyroid cancer.
As demonstrated in the table below, individuals with stage III and IV disease have a significant risk of dying from thyroid cancer.
The identification of some molecular or DNA abnormalities has led to the development of therapies that target these molecular defects. The first of these agents to negotiate the approval process is vandetanib, a tyrosine kinase inhibitor that targets the RET proto-oncogene, two subtypes of the vascular endothelial growth factor receptor, and the epidermal growth factor receptor.[60] For differentiated thyroid carcinoma, strategies are evolving to use selected types of targeted therapy to increase radioactive iodine uptake in papillary thyroid carcinomas that have lost the ability to concentrate iodide. This strategy would make possible the use of radioactive iodine therapy to treat "resistant" thyroid cancers.
Mitogen-activated protein kinase (MAPK) variants are the most common genetic variants seen in thyroid cancer.[10] The BRAF 600E genetic variant is seen in 60% of papillary thyroid cancers. It is associated with increased risks of cervical lymph node metastasis, blunted response to radioactive iodine, and increased rates of local recurrence.[10] RasGTPase mutations are seen in 13% of papillary and 25-50% of follicular cancers and are associated with increased risk of vascular invasion and higher response to radioactive iodine.[10]
Prognosis is better in younger people than older ones.[59]
Prognosis depends mainly on the type of cancer and cancer stage.
| Thyroid cancer type |
5-year survival | 10-year survival | ||||
|---|---|---|---|---|---|---|
| Stage I | Stage II | Stage III | Stage IV | Overall | Overall | |
| Papillary | 100%[61] | 100%[61] | 93%[61] | 51%51%[61] | 96%[62] or 97%[63] | 93%[62] |
| Follicular | 100%[61] | 100%[61] | 71%[61] | 50%[61] | 91%[62] | 85%[62] |
| Medullary | 100%[61] | 98%[61] | 81%[61] | 28%[61] | 80%,[62] 83%[64] or 86%[65] | 75%[62] |
| Anaplastic | (always stage IV)[61] | 7%[61] | 7%[61] or 14%[62] | (no data) | ||
Epidemiology
[edit]Thyroid cancer, in 2010, resulted in 36,000 deaths globally up from 24,000 in 1990.[66] Obesity may be associated with a higher incidence of thyroid cancer, but this relationship remains the subject of much debate.[67]
Thyroid cancer accounts for less than 1% of cancer cases and deaths in the UK. Around 2,700 people were diagnosed with thyroid cancer in the UK in 2011, and around 370 people died from the disease in 2012.[68]
However, in South Korea, thyroid cancer was the 5th most prevalent cancer, which accounted for 7.7% of new cancer cases in 2020.[69]
The incidence of thyroid cancer in the United States increased by 313% from a 1974-1977 incidence of 4.6 cases per 100,000 people to 14.4 cases per 100,000 people in 2010-13.[70] This increase is thought to be due to more widespread use of head and neck imaging (which may incidentally detect thyroid masses) as well as increased use of fine needle aspiration biopsies.[10]
Notable cases
[edit]- Callum Ainley, English footballer[71]
- Ann-Katrin Berger, German women footballer
- Emre Can, German footballer[72]
- Jerry Dipoto, former Major League Baseball pitcher[73]
- Roger Ebert, American film critic
- Jennifer Grey, American actress
- Uhm Jung-hwa, South Korean singer, actress and dancer [74]
- Lee Moon-sae, South Korean ballad singer[75]
- Joe Piscopo, American actor
- Vladimir Putin, president of Russia[76]
- William Rehnquist, Chief Justice of the United States (1986–2005) died September 3, 2005, from anaplastic thyroid cancer[77]
- Katee Sackhoff, American actress
- Karen Smyers, American swimmer
- Daniel Snyder, American owner of the Washington Football Team[78]
- Rod Stewart, British singer
- Scott Thompson, American businessman
- Sofía Vergara, American actress
- Julia Volkova, Russian singer
- April Winchell, American actress
References
[edit]- ^ a b c d e f g h i j "Thyroid Cancer Treatment". National Cancer Institute. 27 April 2017. Archived from the original on 15 July 2017. Retrieved 18 July 2017.
- ^ a b Carling T, Udelsman R (2014). "Thyroid cancer". Annual Review of Medicine. 65: 125–137. doi:10.1146/annurev-med-061512-105739. PMID 24274180.
- ^ a b Shin A, et al. (2022). "Body Mass Index and Thyroid Cancer Risk: A Pooled Analysis of Half a Million Men and Women in the Asia Cohort Consortium". Thyroid. 32 (3): 306–314. doi:10.1089/thy.2021.0445. PMC 8971972. PMID 34915752.
- ^ a b c d e f "Thyroid Cancer Treatment". National Cancer Institute. 12 May 2017. Archived from the original on 16 July 2017. Retrieved 18 July 2017.
- ^ a b c d "Cancer of the Thyroid - Cancer Stat Facts". seer.cancer.gov. Archived from the original on 15 July 2017. Retrieved 18 July 2017.
- ^ a b Vos, Theo; et al. (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ^ a b Wang, Haidong; et al. (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ "Cancer Fact sheet N°297". World Health Organization. February 2014. Archived from the original on 29 December 2010. Retrieved 10 June 2014.
- ^ "Defining Cancer". National Cancer Institute. 17 September 2007. Archived from the original on 25 June 2014. Retrieved 10 June 2014.
- ^ a b c d e f g h i j k l m n Boucai, Laura; Zafereo, Mark; Cabanillas, Maria E. (6 February 2024). "Thyroid Cancer: A Review". JAMA. 331 (5): 425. doi:10.1001/jama.2023.26348.
- ^ Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. (May 2017). "Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 317 (18): 1882–1887. doi:10.1001/jama.2017.4011. PMID 28492905. S2CID 205091526.
- ^ a b World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.15. ISBN 978-9283204299.
- ^ Paz-Pacheco, Elizabeth; Juan, Mari Des San (2 March 2023). "Incidence, Recurrence and Mortality Among Filipinos With Differentiated Thyroid Cancer: A Systematic Review". Journal of the ASEAN Federation of Endocrine Societies. 38 (1): 100–107. doi:10.15605/jafes.038.01.14. PMC 10213166. PMID 37252408.
Nguyen, Michelle Linh T.; Hu, Jiaqi; Hastings, Kattherine G.; Daza, Eric J; Cullen, Mark R.; Orloff, Lisa A.; Palaniappan, Latha P. (7 September 2017). "Thyroid cancer mortality higher in Filipinos in United States: an analysis using national mortality records from 2003–2012". Cancer. 123 (24): 4860–4867. doi:10.1002/cncr.30958. PMC 5716919. PMID 28881423.
Lee, Alice W.; Mendoza, Roy A.; Aman, Shehla; Jsu, Robert; Liu, Lihua (February 2022). "Thyroid cancer incidence disparities among ethnic Asian American populations, 1990–2014". Annals of Epidemiology. 66: 28–36. doi:10.1016/j.annepidem.2021.11.002. PMID 34774744. S2CID 244033542. - ^ a b c d Hu MI, Vassilopoulou-Sellin R, Lustig R, Lamont JP, eds. (2008). "Thyroid and Parathyroid Cancers". Cancer Management: A Multidisciplinary Approach (11th ed.). Lawrence, Kansas: CMP Media. ISBN 978-1-891483-62-2. Archived from the original on 28 February 2010.
- ^ Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS (March 2018). "The Diagnosis and Management of Thyroid Nodules: A Review". JAMA. 319 (9): 914–924. doi:10.1001/jama.2018.0898. PMID 29509871. S2CID 5042725.
- ^ "Thyroid Cancer". Herbert Irving Comprehensive Cancer Center (HICCC) - New York. 1 February 2021. Archived from the original on 5 February 2023. Retrieved 5 February 2023.
- ^ Grani, Giorgio; Sponziello, Marialuisa; Filetti, Sebastiano; Durante, Cosimo (16 August 2024). "Thyroid nodules: diagnosis and management". Nature Reviews Endocrinology. doi:10.1038/s41574-024-01025-4. ISSN 1759-5029.
- ^ "Thyroid Cancer Overview - Signaling Pathway. Diagnosis. Targeted Therapy - Creative Biolabs". www.creativebiolabs.net. Archived from the original on 5 February 2023. Retrieved 5 February 2023.
- ^ "Radioactive I-131 from Fallout". National Cancer Institute. Archived from the original on 19 May 2014. Retrieved 9 June 2014.
- ^ a b dos Santos Silva I, Swerdlow AJ (February 1993). "Thyroid cancer epidemiology in England and Wales: time trends and geographical distribution". British Journal of Cancer. 67 (2): 330–340. doi:10.1038/bjc.1993.61. PMC 1968194. PMID 8431362.
- ^ "Experts link higher incidence of children's cancer to Fukushima radiation". ScienceAlert. 12 October 2015. Archived from the original on 19 January 2016. Retrieved 15 January 2016.
- ^ Pacini F, Castagna MG, Brilli L, Pentheroudakis G (May 2010). "Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up". Annals of Oncology. 21 (Suppl 5): v214–v219. doi:10.1093/annonc/mdq190. PMID 20555084.
- ^ "Genetics of Endocrine and Neuroendocrine Neoplasias". National Cancer Institute. 1 January 1980. Archived from the original on 4 July 2014. Retrieved 9 June 2014.
- ^ Floridi C, Cellina M, Buccimazza G, Arrichiello A, Sacrini A, Arrigoni F, et al. (September 2019). "Ultrasound imaging classifications of thyroid nodules for malignancy risk stratification and clinical management: state of the art". Gland Surgery. 8 (Suppl 3): S233–S244. doi:10.21037/gs.2019.07.01. PMC 6755949. PMID 31559190.
- ^ Bennedbaek FN, Perrild H, Hegedüs L (March 1999). "Diagnosis and treatment of the solitary thyroid nodule. Results of a European survey". Clinical Endocrinology. 50 (3): 357–363. doi:10.1046/j.1365-2265.1999.00663.x. PMID 10435062. S2CID 21514672.
- ^ "Thyroid scan: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 27 January 2021. Retrieved 5 February 2021.
- ^ "Vol 7 Issue 6 p.3-4". American Thyroid Association. Archived from the original on 4 December 2020. Retrieved 5 February 2021.
- ^ Renuka IV, Saila Bala G, Aparna C, Kumari R, Sumalatha K (December 2012). "The bethesda system for reporting thyroid cytopathology: interpretation and guidelines in surgical treatment". Indian Journal of Otolaryngology and Head and Neck Surgery. 64 (4): 305–311. doi:10.1007/s12070-011-0289-4. PMC 3477437. PMID 24294568.
- ^ Gerard SK, Cavalieri RR (January 2002). "I-123 diagnostic thyroid tumor whole-body scanning with imaging at 6, 24, and 48 hours". Clinical Nuclear Medicine. 27 (1): 1–8. doi:10.1097/00003072-200201000-00001. PMID 11805475. S2CID 22871325.
- ^ Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. (May 2017). "Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 317 (18): 1882–1887. doi:10.1001/jama.2017.4011. PMID 28492905. S2CID 205091526.
- ^ Malith V, Bombil I, Harran N, Luvhengo TE (September 2018). "Demographic and histological subtypes of Hurthle cell tumours of the thyroid in a South African setting". South African Journal of Surgery. Suid-Afrikaanse Tydskrif vir Chirurgie. 56 (3): 20–23. doi:10.17159/2078-5151/2018/v56n3a2557 (inactive 24 April 2024). PMID 30264938.
{{cite journal}}: CS1 maint: DOI inactive as of April 2024 (link) - ^ "Thyroid Cancer Treatment". National Cancer Institute. 1 January 1980. Archived from the original on 21 April 2008. Retrieved 22 December 2007.
- ^ "Thyroid cancer". National Cancer Institute. Archived from the original on 20 December 2007. Retrieved 22 December 2007.
- ^ a b c Chapter 20 in: Mitchell RS, Kumar V, Abbas AK, Fausto N (2007). Robbins Basic Pathology. Philadelphia: Saunders. ISBN 978-1-4160-2973-1. 8th edition.
- ^ Yu XM, Schneider DF, Leverson G, Chen H, Sippel RS (October 2013). "Follicular variant of papillary thyroid carcinoma is a unique clinical entity: a population-based study of 10,740 cases". Thyroid. 23 (10): 1263–1268. doi:10.1089/thy.2012.0453. PMC 3787730. PMID 23477346.
- ^ Grani G, Lamartina L, Durante C, Filetti S, Cooper DS (June 2018). "Follicular thyroid cancer and Hürthle cell carcinoma: challenges in diagnosis, treatment, and clinical management". The Lancet. Diabetes & Endocrinology. 6 (6): 500–514. doi:10.1016/S2213-8587(17)30325-X. PMID 29102432. S2CID 24129533.
- ^ Schlumberger M, Carlomagno F, Baudin E, Bidart JM, Santoro M (January 2008). "New therapeutic approaches to treat medullary thyroid carcinoma". Nature Clinical Practice. Endocrinology & Metabolism. 4 (1): 22–32. doi:10.1038/ncpendmet0717. PMID 18084343. S2CID 25818628.
- ^ "Anaplastic Thyroid Cancer". Columbia Thyroid Center. Archived from the original on 23 December 2019. Retrieved 30 March 2020.
- ^ Nix P, Nicolaides A, Coatesworth AP (December 2005). "Thyroid cancer review 2: management of differentiated thyroid cancers". International Journal of Clinical Practice. 59 (12): 1459–1463. doi:10.1111/j.1368-5031.2005.00672.x. PMID 16351679. S2CID 7912705. Archived from the original on 20 May 2013.
- ^ Nix PA, Nicolaides A, Coatesworth AP (January 2006). "Thyroid cancer review 3: management of medullary and undifferentiated thyroid cancer". International Journal of Clinical Practice. 60 (1): 80–84. doi:10.1111/j.1742-1241.2005.00673.x. PMID 16409432. S2CID 11825588.
- ^ Shaha AR (May 2007). "TNM classification of thyroid carcinoma". World Journal of Surgery. 31 (5): 879–887. doi:10.1007/s00268-006-0864-0. PMID 17308849. S2CID 23121159.
- ^ Dideban S, Abdollahi A, Meysamie A, Sedghi S, Shahriari M (2016). "Thyroid Papillary Microcarcinoma: Etiology, Clinical Manifestations, Diagnosis, Follow-up, Histopathology and Prognosis". Iranian Journal of Pathology. 11 (1): 1–19. PMC 4749190. PMID 26870138.
- ^ Hughes DT, Haymart MR, Miller BS, Gauger PG, Doherty GM (March 2011). "The most commonly occurring papillary thyroid cancer in the United States is now a microcarcinoma in a patient older than 45 years". Thyroid. 21 (3): 231–236. doi:10.1089/thy.2010.0137. hdl:2027.42/90466. PMID 21268762.
- ^ Woolner LB, Lemmon ML, Beahrs OH, Black BM, Keating FR (January 1960). "Occult papillary carcinoma of the thyroid gland: a study of 140 cases observed in a 30-year period". The Journal of Clinical Endocrinology and Metabolism. 20: 89–105. doi:10.1210/jcem-20-1-89. PMID 13845950.
- ^ "Cancer Staging - NCI". www.cancer.gov. 9 March 2015. Archived from the original on 19 March 2015. Retrieved 5 February 2023.
- ^ Hindié E, Zanotti-Fregonara P, Keller I, Duron F, Devaux JY, Calzada-Nocaudie M, et al. (September 2007). "Bone metastases of differentiated thyroid cancer: impact of early 131I-based detection on outcome". Endocrine-Related Cancer. 14 (3): 799–807. doi:10.1677/ERC-07-0120. PMID 17914109.
- ^ Schlumberger M, Arcangioli O, Piekarski JD, Tubiana M, Parmentier C (November 1988). "Detection and treatment of lung metastases of differentiated thyroid carcinoma in patients with normal chest X-rays". Journal of Nuclear Medicine. 29 (11): 1790–1794. PMID 3183748.
- ^ Das S (2008). A concise textbook of surgery (5th ed.). Calcutta: Dr S. Das. ISBN 978-8190568128.
- ^ a b Cooper DS, Doherty GM, Haugen BR, Hauger BR, Kloos RT, Lee SL, et al. (November 2009). "Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer". Thyroid. 19 (11): 1167–1214. doi:10.1089/thy.2009.0110. hdl:2027.42/78131. PMID 19860577.
- ^ British Thyroid Association, Royal College of Physicians, Perros P (2007). Guidelines for the management of thyroid cancer. 2nd edition. Report of the Thyroid Cancer Guidelines Update Group (PDF). Royal College of Physicians. p. 16. ISBN 9781860163098. Archived from the original (PDF) on 26 December 2011. Retrieved 12 July 2013.
- ^ Haugen, Bryan R.; Alexander, Erik K.; Bible, Keith C.; Doherty, Gerard M.; Mandel, Susan J.; Nikiforov, Yuri E.; Pacini, Furio; Randolph, Gregory W.; Sawka, Anna M.; Schlumberger, Martin; Schuff, Kathryn G.; Sherman, Steven I.; Sosa, Julie Ann; Steward, David L.; Tuttle, R. Michael; Wartofsky, Leonard (January 2016). "2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer". Thyroid. 26 (1): 1–133. doi:10.1089/thy.2015.0020.
- ^ Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. (January 2016). "2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer". Thyroid. 26 (1): 1–133. doi:10.1089/thy.2015.0020. PMC 4739132. PMID 26462967.
- ^ Wells SA, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, et al. (American Thyroid Association Guidelines Task Force on Medullary Thyroid Carcinoma) (June 2015). "Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma". Thyroid. 25 (6): 567–610. doi:10.1089/thy.2014.0335. PMC 4490627. PMID 25810047.
- ^ Smallridge RC, Ain KB, Asa SL, Bible KC, Brierley JD, Burman KD, et al. (November 2012). "American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer". Thyroid. 22 (11): 1104–1139. doi:10.1089/thy.2012.0302. PMID 23130564.
- ^ Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. (July 2014). "Guidelines for the management of thyroid cancer". Clinical Endocrinology. 81 (Suppl 1): 1–122. doi:10.1111/cen.12515. PMID 24989897.
- ^ a b Lamartina L, Grani G, Durante C, Filetti S (18 January 2018). "Recent advances in managing differentiated thyroid cancer". F1000Research. 7: 86. doi:10.12688/f1000research.12811.1. PMC 5773927. PMID 29399330.
- ^ a b c Welch HG, Schwartz L, Woloshin S (2011). Overdiagnosed: Making People Sick in the Pursuit of Health. [Malaysia?]: Beacon Press. pp. 61–34. ISBN 978-0-8070-2200-9.
- ^ "Thyroid Cancer". MedicineNet.com. Archived from the original on 20 October 2011. Retrieved 26 October 2011.
- ^ a b Numbers from EUROCARE, from Page 10 Archived 13 May 2016 at the Wayback Machine in: Grünwald F, Biersack HJ (2005). Thyroid cancer. Berlin: Springer. ISBN 978-3-540-22309-2.
- ^ "FDA approves new treatment for rare form of thyroid cancer" (Press release). U.S. Food and Drug Administration. 6 April 2011. Archived from the original on 10 April 2011. Retrieved 7 April 2011.
- ^ a b c d e f g h i j k l m n o cancer.org Thyroid Cancer Archived 18 October 2013 at the Wayback Machine By the American Cancer Society. In turn citing: AJCC Cancer Staging Manual (7th ed).
- ^ a b c d e f g Numbers from National Cancer Database in the US, from Page 10 Archived 13 May 2016 at the Wayback Machine in: Grünwald F, Biersack HJ (2005). Thyroid cancer. Berlin: Springer. ISBN 978-3-540-22309-2. (Note:Book also states that the 14% 10-year survival for anaplastic thyroid cancer was overestimated)
- ^ Rounded up to nearest natural number from 96.7% as given by Santacroce L, Gagliardi S, Kennedy AS (28 September 2010). "Thyroid, Papillary Carcinoma". eMedicine. Archived from the original on 28 July 2010.
- ^ By 100% minus cause-specific mortality of 17% at 5 yr, as given by Barbet J, Campion L, Kraeber-Bodéré F, Chatal JF (November 2005). "Prognostic impact of serum calcitonin and carcinoembryonic antigen doubling-times in patients with medullary thyroid carcinoma". The Journal of Clinical Endocrinology and Metabolism. 90 (11): 6077–6084. doi:10.1210/jc.2005-0044. PMID 16091497.
- ^ "Medullary Thyroid Cancer". National Cancer Institute. 4 February 2016. Archived from the original on 30 May 2016. Retrieved 11 May 2016.
- ^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–2128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMC 10790329. PMID 23245604. S2CID 1541253.
- ^ Santini F, Marzullo P, Rotondi M, Ceccarini G, Pagano L, Ippolito S, et al. (October 2014). "Mechanisms in endocrinology: the crosstalk between thyroid gland and adipose tissue: signal integration in health and disease". European Journal of Endocrinology. 171 (4): R137–R152. doi:10.1530/eje-14-0067. PMID 25214234. Archived from the original on 11 November 2014.
- ^ "Thyroid cancer statistics". Cancer Research UK. Archived from the original on 17 October 2014. Retrieved 28 October 2014.
- ^ "Republic of Korea Cancer Rates" (PDF). Global Cancer Observatory (GCO). World Health Organization. 2020. Archived (PDF) from the original on 11 November 2022. Retrieved 5 February 2022.
- ^ Lim, Hyeyeun; Devesa, Susan S.; Sosa, Julie A.; Check, David; Kitahara, Cari M. (4 April 2017). "Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013". JAMA. 317 (13): 1338. doi:10.1001/jama.2017.2719.
- ^ "Callum Ainley: Grimsby Town midfielder diagnosed with thyroid cancer". BBC Sport. 16 January 2024. Retrieved 17 January 2024.
- ^ Hunsley, James (27 January 2023). "'I am so grateful' - ex-Liverpool midfielder Emre Can opens up on battle with cancer". Goal.com. Archived from the original on 28 January 2023. Retrieved 29 January 2023.
- ^ Bamberger, Michael (27 May 2002). "Survivors". Sports Illustrated. Archived from the original on 1 March 2014. Retrieved 11 August 2013.
- ^ "Uhm Jung-hwa had Thyroid cancer op". The Korean Herald. 20 October 2010. Archived from the original on 5 February 2022. Retrieved 5 February 2022.
- ^ "Lee Moon-se risks cancer relapse to keep singing". The Korean Herald. 31 March 2015.
- ^ Jacobs E (3 April 2022). "Putin under care of cancer doctor, bathing in deer antler blood: Report". Washington Examiner. Archived from the original on 3 April 2022. Retrieved 3 April 2022.
- ^ Lane C (8 September 2005). "Rehnquist Eulogies Look Beyond Bench". The Washington Post. Archived from the original on 4 March 2016. Retrieved 11 May 2016.
- ^ "Celebrities with Thyroid problems". Alexander Shifrin. Archived from the original on 26 August 2013. Retrieved 11 August 2013.
External links
[edit]- Thyroid cancer at Curlie
- Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer—The American Thyroid Association Guidelines Taskforce (2015)
- Common sites where thyroid cancer metastasizes.